Diabetic retinopathy is a common condition affecting about 4 million Americans. It is the most common cause of severe vision loss in the population under age 60. The likelihood of having diabetic retinopathy increases with the number of years being diabetic, with 60% of adult onset diabetics and 95% of juvenile onset diabetics having retinopathy after 20 years. Blood sugar can damage the walls of the fine blood vessels of the retina, causing leakage and sometimes permanent loss of blood vessels. The full spectrum of diabetic retinopathy is divided into nonproliferative and proliferative diabetic retinopathy.
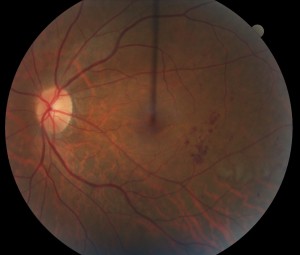
Photo of Nonproliferative diabetic retinopathy
Nonproliferative diabetic retinopathy (NPDR) is the more common and typically less severe stage of diabetic retinopathy. It is subclassified into mild, moderate, and severe NPDR with each levels at a progressively more likely to develop high risk disease. NPDR is characterized by the presence of small hemorrhages and changes to the blood vessels of the retina. It can occur with or without edema (swelling) of the macula. For the most part, nonproliferative diabetic retinopathy is observed, although injections of medication and/or laser is typically performed if there is significant macular edema. Injections and/or laser can also be used in cases of severe NPDR, especially if there is a significant possibility of developing high risk disease.
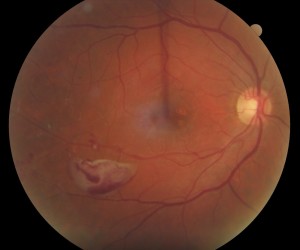
Photo of Proliferative diabetic retinopathy
Proliferative diabetic retinopathy (PDR) is the more severe stage of diabetic retinopathy. It is characterized by the presence of abnormal blood vessel growth (neovascularization) which is fueled by ischemia (lack of circulation) to portions of the retina. Neovascularization in turn causes severe bleeding and eventually scarring of the retina and frequent results in severe vision loss. Proliferative diabetic retinopathy is treated with panretinal laser and injections of medication. A surgery called vitrectomy is often performed in hopes of stabilizing or improving vision.
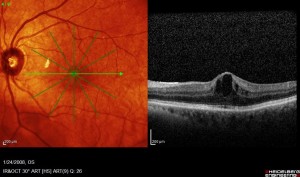
Photo and OCT of Diabetic macular edema
Diabetic macular edema (DME) may occur with either NPDR of all severity levels or PDR. It is the most common cause of blurry vision associated with diabetic retinopathy. It occurs when the blood vessels in and near the macula leak clear fluid and lipid. This process may cause the tissue of the macula to become swollen with resultant loss of vision. It is treated with injections of anti-VEGF (vascular endothelial growth factor) medication, corticosteroids, and/or laser.